ME/CFS
ME/CFS is a physical disorder. There are definite symptoms and physical findings associated with the disease.
ME/CFS is NOT a psychological condition although there may be emotional overtones as a result of the disease. Such emotional overtones can add to the complexity of a sufferer’s condition as well the clinician’s diagnosis.
ME/CFS is not depression. In general, people who suffer from ME/CFS tend to overestimate their abilities, retain a strong interest in life and respond poorly to exercise. The opposite is typically observed in people with depression. Nonetheless, some patients with ME/CFS can get “secondary depression” because of losses related to the condition such as employment, the ability to take care of oneself, and social/ family life.
ME/CFS is characterized by unexplained, persistent or recurrent physical and cognitive collapses in which the body and mind are unable to function at normal levels.
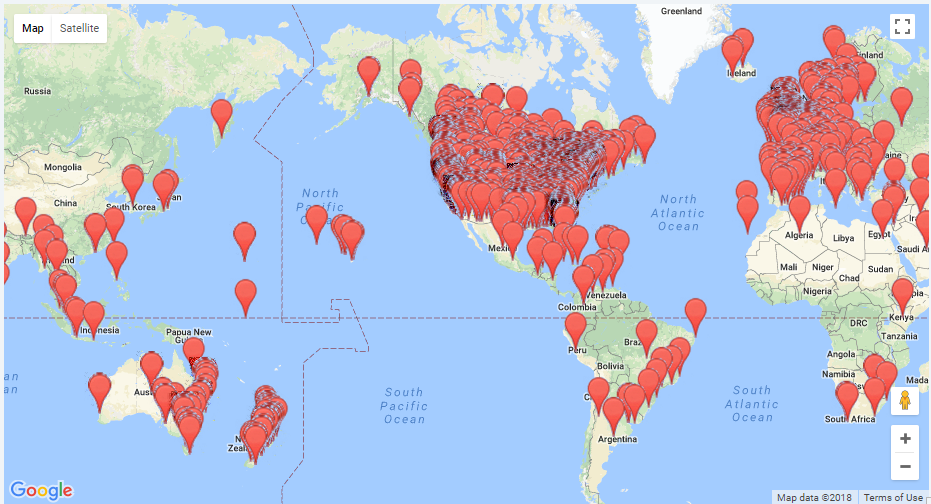
Studies reveal an ME/CFS prevalence rate of .042% of the general population which makes it significantly more prevalent than multiple sclerosis, cerebral palsy and muscular dystrophy combined. Over 28,000,000 individuals are afflicted worldwide and women suffer its ravages far more than men.
This condition has been terribly mislabeled as Chronic Fatigue Syndrome (CFS) in much of North America. In other parts of the world, the more comprehensive term Myalgic Encephalomyelitis (M.E.) is most commonly used for the illness.
The CFS label is misleading because profound fatigue is only one of a constellation of symptoms associated with the condition as noted below. What has been referred to as fatigue is much more closely akin to a dramatic collapse of both physical and cognitive abilities.
Those who are severely ill with ME/CFS function at a level lower than someone undergoing chemotherapy or someone who has heart disease.
The following is a list of some of the symptoms commonly associated with ME/CFS as drawn from the Canadian Physicians Consensus Manual on the disease. To be clinically diagnosed as having ME/CFS, the condition must be present for at least six months or more, not made better by rest and accompanied by six or more of the following symptoms:
Post-exertional malaise lasting 24 hours or more:
After relatively normal physical or intellectual exertion, a patient may take an inordinate amount of time to regain her/his pre-exertion level of function and competence. This reactive state usually lasts 24 hours or more.
Sleep Dysfunctions:
Sleep disturbances may include early, middle or late insomnia, with reversed or irregular insomnia and over sleeping. Loss of the deeper phases of sleep is especially characteristic, with frequent awakenings, and loss of restorative feelings in the morning.
Abdominal Complaints:
Abdominal complaints such as discomfort, pain and abnormal bowel movements.
Widespread Pain:
Pain is often generalized and occurs in unexpected places at unexpected times. The pains may be sharp, shooting, burning or aching. More frequent, severe or newer types of headaches are also possible. Please note: Pain that is progressive, particularly if it wakes up a patient, requires immediate attention by a Physician.
Neurological Dysfunctions:
The neurological/cognitive symptoms are more characteristically variable than constant and often have a distinct fatiguing component to them. Especially common are cognitive ‘fog’ or confusion, slowed information processing speed, trouble with word retrieval and speaking or intermittent dyslexia, trouble with writing, reading, and mathematics, and short-term memory loss.
Perceptual Disturbances:
A reduced ability to make figure/ground distinctions, loss of depth perception or inability to focus vision and attention.
Motor Disturbances:
Muscle weakness, loss of balance and clumsiness.
Orthostatic Intolerance:
Disturbances in the regulation of blood pressure and pulse; autonomic disorders such as difficulties with balance and standing.
Immune Dysfunctions:
Some sufferers may exhibit symptoms coming from immune system activation. There is often general malaise–flu like feelings of being ‘ill’ and feeling feverish. new sensitivities to medications and/or various chemicals can develop.
Leading scientific researchers believe there may ultimately prove to be dozens of different sub-sets of the disease which are currently grouped together for lack of clear bio-markers which can be identified through testing.
One result of the current lack of knowledge on the disease is that it is all too often misdiagnosed by far too many physicians and frequently, improperly treated. Expert medical advise is extremely limited. It is estimated that perhaps only as few as 17% of those afflicted have been properly diagnosed.
For more medically specific information about ME/CFS you may wish to consult:
Fakuda Case Definition (https://www.acpjournals.org/doi/10.7326/0003-4819-121-12-199412150-00009)
For more first hand information directly from the those who suffer from ME/CFS (https://ME-CFSCommunity.com)